
THE PLAN’S FIVE PRIORITY AREAS
The plan for each priority area is described in the following sections.The RBA process requires the workgroups to select only a handful of indicators (less than five indicators each) in order to better focus community efforts on making an impact on population health.The workgroups found it difficult to select the most important issues to work on over the next three years, because several other health issues are also important. Each workgroup’s final decisions are presented next, including their results statements, indicators, root causes, and strategies to move the needle on population health.
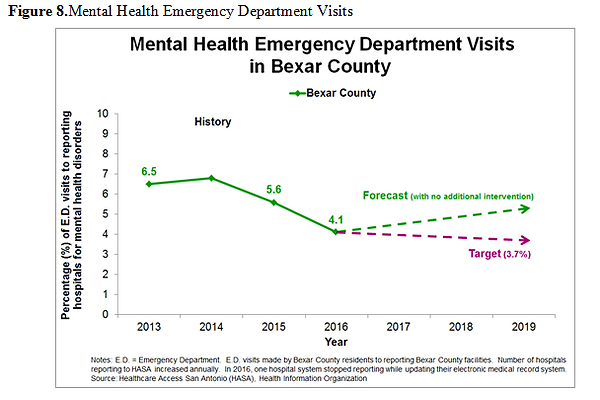
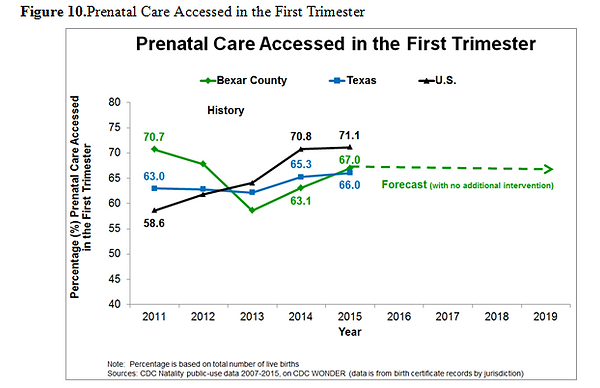
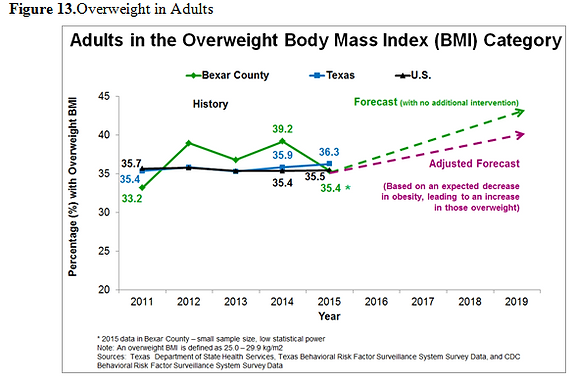
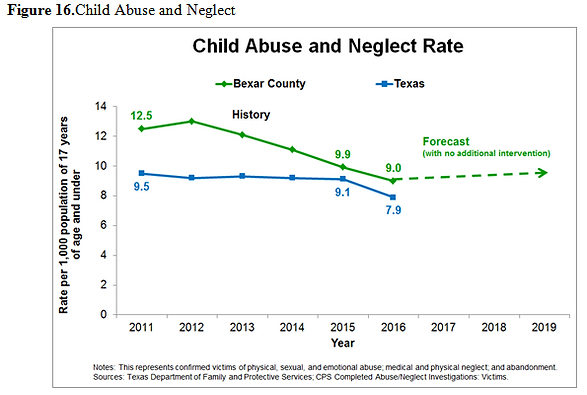
Graphs for each headline indicator are also presented. National data are presented in black; Texas data are presented in blue. Values for Bexar County data are in green. The green forecast lines also show what can be expected of this trend by 2019 if no additional intervention is implemented. The pink lines in the graphs display the workgroups’ targets or where they expect this value to be by 2019, in part due to their population health strategies and actions. As of October 2017, some workgroups were still setting their targets for their headline indicators.
A.BEHAVIORAL AND MENTAL WELL-BEING
Why is this important?
Behavioral health issues, consisting of mental health and substance-related disorders, are associated with family violence, chronic medical conditions, and premature death (Substance Abuse and Mental Health Services Administration, 2017; Surgeon General, 2017). Managing and treating behavioral health issues can lead to behavioral and mental well-being, which is essential for overall health. Behavioral and mental well-being can help individuals realize their full potential, cope with life stresses, work productively, and contribute significantly to their communities.
Results Statement
The Bexar County community is committed to hope and recovery through open conversations on emotional wellness, substance-related disorder and mental health, by providing integrated preventive care and clinical treatment that is community based and family and youth guided.
Headline Indicators
-
Mental health emergency department visits
-
Substance-related disorders emergency department visits
Story Behind the Baseline
Carol and Ted[1] were completely taken by surprise when they found the suicide notes left by their 14-year old son. At a loss about what to do, they took him to the emergency department(ED) where he was kept for 16 hours with no psychiatric support while waiting for a bed in a community psychiatric hospital. Finally, their child was transported to a local hospital where he was assessed and received initial care. This story illustrates what is happening in Bexar County: the surprising prevalence of behavioral health issues among youth and adults, the fact that too often the illness is not detected nor treated early enough because of stigma and/or the difficulty in finding mental health or substance-related disorder services, and the fact that these cases end up in ED settings which are often not equipped to treat them.
Prevalence of Behavioral Health Issues
According to the 2016 National Survey on Drug Use and Health, approximately 44.7 million American adults or 18.3 percent of the adult population aged 18 or older had a mental illness in the past year (Substance Abuse and Mental Health Services Administration, 2016). In 2010, rates among children were comparable with one in five children in the United States having a mental health disorder, which impairs how they function at home, school, or in the community (Office of Disease Prevention and Health Promotion, 2014). The 2016 survey also revealed that 20.1 million people or 7.5 percent of people aged 12 or older experienced a substance-related disorder in the past year, including an alcohol disorder and an illicit drug use disorder, such as opioid abuse (Substance Abuse and Mental Health Services Administration, 2016). This percentage represents approximately 4.3 percent of youths aged 12 to 17, 15.1 percent of young adults aged 18 to 25, and 6.6 percent of adults aged 26 or older (Substance Abuse and Mental Health Services Administration, 2016).Substance-related disorders often co-occur with mental illness. People with mental illness often self-medicate with substances such as alcohol and other drugs (Khantzian, 2013; Suh, Ruffins, Robins, Albanese, & Khantzian, 2008). It is also common that children or adults have more than one mental health disorder (Office of Disease Prevention and Health Promotion, 2014).
Texas data follow the national story, with 16.9 percent of all adults experiencing mental health challenges, and 8.0 percent of adults having substance-related disorders (Mental Health America, 2017).
In Bexar County, nearly 60,000 adults or 3.2 percent of adults in 2015 were suffering from a serious mental illness and 37,500 Bexar County children or 2.0 percent of children experienced serious emotional disturbance (The Meadows Mental Health Policy Institute, & Methodist Healthcare Ministries of South Texas, Inc., 2016).
The Use of Emergency Departments
An unintended consequence of the lack of mental health and substance-related disorder care in our community is the increase in emergency department (ED) visits by adults, children, and teens with behavioral health challenges. (Please note that Figures 7 and 8 do not show an annual increase in ED visits because of the addition of new hospitals reporting to the health information exchange. The data would show an increase in ED visits if no new hospital was added.) Individuals access the ED when the behavioral health issue is at a high level of acuity, indicating absent or insufficient previous care, and when all other solutions are unaffordable. Among Bexar County adults alone, 22,087 ED visits took place in 2015 for adults experiencing a mental health crisis or a substance-related disorder (The Meadows Mental Health Policy Institute, & Texas Conference of Urban Counties, 2015).A person presenting at the ED for behavioral health reasons may not receive the care he/she needs including emergency mental health assessments or follow-up outpatient mental health care (Clarity Child Guidance Center, 2013). In addition, accessing the ED to treat mental health and substance-related disorders is the most expensive and ineffective option for community residents. Some community solutions exist to divert frequent ED users, such as the San Antonio Fire Department Mobile Integrated Healthcare (City of San Antonio, 2017). However, greater efforts are needed to address the root causes of behavioral health ED visits.
Based on reported hospital data in 2016, 4.1% of all Bexar County ED visits were for mental health issues, while 9.7% of all ED visits were for substance-related disorders (Healthcare Access San Antonio, 2017). Both of these are expected to increase in Bexar County without additional intervention. By 2019, the partners that are working on mental health disorders are expecting the percentage of ED visits to decrease to 3.7 percent.
Three Prioritized Root Causes that Impact ED Visits
Three root causes that may help explain the surge in ED visits related to behavioral health were identified and prioritized:
-
There is a lack of service capacity to meet targeted mental health and substance-related disorder needs in Bexar County. There are severe psychiatric bed shortages in Texas (Torrey, Entsminger, Geller, Stanley, & Jaffe, 2008) and in Bexar County (Clarity Child Guidance Center, 2013), and the needs for inpatient mental health and substance-related disorder admissions are increasing (Health Care Cost Institute, 2012). Outpatient services are also lacking, where the wait time for an initial appointment with a psychiatrist is between 3 to 6 months (Clarity Child Guidance Center, 2013; Department of State Health Services, 2014).
-
Another root cause of ED use is limited education regarding mental health and substance-related disorders. Family members, school officials, clergy, businesses all need education about recognizing signs that someone needs help, where to go when resources are needed, and learning how to navigate the behavioral health care system. Providing such education can help decrease potential stigma such as unwarranted assumptions, distrust, avoidance, pity, and gossip that people with mental illness often experience (Moses, 2010). Requiring mandatory screenings for mental health and substance-related disorders in schools may also help raise awareness and promote early detection, thus reducing ED visits.
-
A third root cause is a lack of coordinated care between primary care providers and behavioral health specialists in Bexar County. Providers may use different information technology systems, along with the Health Insurance Portability and Accountability Act, making the dissemination of patient information difficult across systems. In addition, cross-payer and cross-agency collaborationsmay be limited resulting in limited countywide policies, procedures, and metrics for children and adults with behavioral health issues.
Prioritized Root Causes for the Community to Address
-
Lack of behavioral (mental health and substance-related disorders)health service capacity
-
Lack of overarching education about behavioral (mental health and substance-related disorders) health
-
Lack of levels of care or coordinated behavioral (mental health and substance-related disorders) care
Key Strategies
-
Promote building blocks for a community wide system of care.
-
Create a community wide awareness and education plan.
-
Facilitate telemedicine for behavioral health in Bexar County, including mental health and substance-related disorders in primary care settings.
-
Increase interest in behavioral (mental health and substance-related disorders) health training and careers across professions.
References
City of San Antonio. (2017). Mobile integrated healthcare pilot program. Retrieved from http://www.sanantonio.gov/SAFD/About/Divisions/Emerency-Medical-Services/MobileHealthcare
Clarity Child Guidance Center. (2013). The state of children’s mental health in Bexar County. Retrieved from
http://www.texasrhp6.com/wp-content/uploads/2014/01/GapAssessmentFINAL_20130828.pdf
Department of State Health Services. (2014). The mental health workforce shortage in Texas. Retrieved from
https://www.dshs.texas.gov/legislative/2014/Attachment1-HB1023-MH-Workforce-Report-HHSC.pdf
Healthcare Access San Antonio. (2017). Analysis provided by Healthcare Access San Antonio.
Health Care Cost Institute. (2012). Health care cost and utilization report: 2010. Retrieved from http://www.healthcostinstitute.org/wp-content/uploads/2016/11/HCCI_HCCUR2010.pdf
Khantzian, E. J. (2013). Addiction as a self‐regulation disorder and the role of self‐medication. Addiction, 108(4), 668-669.
Mental Health America. (2017). Mental health in America – Adult data. Retrieved from http://www.mentalhealthamerica.net/issues/mental-health-america-adult-data
Moses, T. (2010). Being treated differently: Stigma experiences with family, peers, and school staff among adolescents with mental health disorders. Social Science & Medicine, 70(7), 985-993.
Office of Disease Prevention and Health Promotion. (2014). Mental health. Retrieved from https://www.healthypeople.gov/2020/leading-health-indicators/2020-lhi-topics/Mental-Health
Substance Abuse and Mental Health Services Administration. (2017). Behavioral Health Treatments and Services. Retrieved from https://www.samhsa.gov/treatment
Substance Abuse and Mental Health Services Administration. (2016). 2016 National survey on drug use and health. Retrieved from https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2016/NSDUH-FFR1-2016.htm#mi1
Suh, J. J., Ruffins, S., Robins, C. E., Albanese, M. J., & Khantzian, E. J. (2008). Self-medication hypothesis: Connecting affective experience and drug choice.Psychoanalytic Psychology, 25(3), 518-532.
Surgeon General. (2017). Mental and emotional well-being. Retrieved from https://www.surgeongeneral.gov/priorities/prevention/strategy/mental-and-emotional-well-being.html
The Meadows Mental Health Policy Institute, & Methodist Healthcare Ministries of South Texas, Inc. (2016). Bexar County mental health systems assessment. Retrieved from http://www.mhm.org/library/bexar-county-mental-health-systems-assessment/download
Torrey, E. F., Entsminger, K., Geller, J., Stanley, J., & Jaffe, D. J. (2008). The shortage of public hospital beds for mentally ill persons. Retrieved from
http://www.treatmentadvocacycenter.org/storage/documents/the_shortage_of_publichospital_beds.pdf
[1] Names changed to protect privacy


B. HEALTHY CHILD AND FAMILY DEVELOPMENT
Why is this important?
Positive early experiences are essential for a child to enjoy a long and healthy life. These experiences start before and during a mother’s pregnancy, and continue through birth, infancy, childhood, and adolescence. Health promotion is crucial to ensure a child growsto be physically, cognitively, socially, and emotionally healthy (Hagan, Shaw, & Duncan, 2008). A child’s development is also influenced by his/her family members’ wellbeing and access to resources, including being able meet their basic needs and having access to services such as child care, education, and health care. Improving the well-being of mothers, infants, and children determines the health of the next generation (Office of Disease Prevention and Health Promotion, 2014)
Results Statement
Bexar County residents will be healthy and have timely access to and utilization of quality resources needed for lifelong success.
Headline Indicators
-
Utilization of preventive primary care measured by:
-
Prenatal care accessed in the first trimester
-
Immunizations in early childhood (<36 months of age)
-
Associated Indicators
-
Prenatal care accessed in the second trimester
-
Prenatal care accessed in the third trimester
-
Not accessing prenatal care
Story Behind the Baseline
Access to preventive primary health care is essential for good health across the life course. It can help detect and prevent serious illnesses and keep individuals healthy, for example, through immunizations and contraception. Establishing a regular primary care provider ensures a continuity of care with a health professional who knows one’s health history, habits, and goals. Despite these benefits, Americans use preventive services at about half the recommended rate (Centers for Disease Control and Prevention, 2013). Texas is featured among the bottom five states where preventative primary care is used (United Health Foundation, 2017).
Two ways to measure utilization of preventive primary care is through access to health care and immunizations (United Health Foundation, 2017). These types of preventive primary care were found to vary by income, race/ethnicity, and education. For example, Hispanics report using preventive services less than non-Hispanic whites and non-Hispanic African Americans (United Health Foundation, 2017). Individuals without health insurance access health care and preventive services less often than individuals with health insurance (Almeida, Dubay, & Ko, 20001; United Health Foundation, 2017). Among populations with health coverage, low-income populations face greater barriers to accessing primary care services because they may not be able to afford their premiums, deductibles and co-payments associated with accessing care, compared to higher income populations. Other important barriers such as language, immigration status, low education, and limited health literacy affect the individual’s ability to effectively navigate the health care system and communicate with providers; these may significantly reduce the likelihood that families will have regular check-ups and immunizations to stay healthy (Centers for Disease Control and Prevention, 2013; Escarce & Kapur, 2006).
When individuals do not have access to a primary care clinic for prevention (e.g., vaccines), acute care (e.g., for colds and flu), or urgent care (e.g., for wheezing or joint pain), they go to the emergency department (ED). However, EDs do not perform preventive measures, but, by definition, are established to address the “ABC’s” (Airway, Breathing, Circulation). As the 1986 Emergency Medical Treatment and Labor Act (EMTALA) states that anybody coming to the ED will be stabilized and treated regardless of their insurance status or ability to pay (Centers for Medicare & Medicaid Services, 2012), ED personnel can only provide temporary care and instruct the individual to follow up with their primary care provider. When these individuals have no such relationship or clinic, they avoid going to the ED until their condition gets worse. The rate of ED visits for non-emergency care is therefore an indication of the population who do not utilize preventive primary care. Medicaid managed care organizations gather this type of information, however, this indicator will not be tracked at this time. The Healthy Child and Family Development workgroup will continue to look for the best way to measure and track ED visits for non-emergency care in the near future.
Preventive primary care also includes regular prenatal care visits for pregnant women to promote the health of the mother and the baby as well as treat and prevent potential health problems during pregnancy (U.S. National Library of Medicine, 2017).Women should schedule a prenatal care visit as soon as they know or suspect that they are pregnant, ideally within the first trimester of pregnancy (U.S. Department of Health and Human Services, 2014). However, close to 40% of Texas women, primarily African American and Hispanic women, receive either late or no prenatal care at all (Texans Care for Children, 2016). No or inadequate prenatal care is more likely to lead to low birth weight babies and pregnancy-related complications (Sunil, Spears, Hook, Castillo, & Torres, 2010).In 2014, more than 1 in 5 pregnant adolescents in Bexar County received no prenatal care (San Antonio Metropolitan Health District, 2017). As of 2015 in Bexar County, 67.0 percent of all live births were from mothers who entered prenatal care in the first trimester, which indicates that one in three mothers did not access prenatal care during these crucial first three months of their pregnancy (U.S. Department of Health and Human Services, 2017). The national Healthy People 2020 goal is that at least 77.9 percent of pregnant women access first trimester prenatal care (Office of Disease Prevention and Health Promotion, 2014). Barriers reported by mothers include lacking information about prenatal care and health insurance such as Medicaid and Children’s Health Insurance Program, having difficulty making appointments, not having enough time, transportation, childcare, and not knowing they are pregnant (San Antonio Metropolitan Health District, 2017).
Immunizations are also an important component of preventive primary care. Vaccines are safe and effective; they protect children, adolescents, and adults from infectious diseases and cancer. Universal immunization prevents disease outbreaks in a community and also protects individuals who cannot be vaccinated due to health reasons (Child Trends Databank, 2015).The majority of vaccines are required in the first three years of a child’s life because many diseases are more common and deadly among infants and small children (Child Trends Databank, 2015). Seven key childhood vaccines are required between 19 and 35 months of age; the combined seven vaccine series is also known as the 4:3:1:3:3:1:4 series which represents the number of recommended doses for each vaccine: four doses of diphtheria-tetanus-acellular pertussis (DTaP), three doses of polio, one dose of measles-mumps-rubella (MMR), three doses of Haemophilus influenza type b (Hib), three doses of hepatitis B (HepB), one dose of varicella, and four doses of the pneumococcal conjugate vaccine (PCV).2015 U.S. data revealed that, on average, 72.2 percent of children between 19 and 35 months of age receive the combined 4:3:1:3:3:1:4 series (Centers for Disease Control and Prevention, 2015).
In Texas, approximately 71.2 percent of young children receive the combined seven vaccine series; however, coverage in Bexar County is below state and national averages with only 67.5 percent of children covered in that age group (Centers for Disease Control and Prevention, 2015). Continuity of care is crucial for children to complete all their required doses, however may be challenging when parents have limited understanding of vaccines, or experience problems with insurance, transportation, or getting time off work to get their child vaccinated (Willis et al., 2016). The rate in Bexar County is expected to decline without additional intervention.
Prioritized Root Causes for the Community to Address
-
Lack of access to health care, especially related to preventive primary car
-
Lack of health literacy as it relates to education, culture, and language
-
Lack of integration and continuity of services including community-based and clinical
Key Strategies
-
Identify, create more, and promote home visiting programs for pregnant and parenting individuals with children up to five years old with less restrictive eligibility criteria and increase linkages of individuals to these services.
-
Provide whole family immunizations at more venues.
-
Develop and promote Patient-Centered Medical Homes (PCMH) where patients are connected to community services and educated about these services by any of the following: community health workers, navigators, case managers, or office practice managers.
-
Develop and connect residents to geographically accessible healthy hubs (e.g., one per area) where families can access medical needs, basic needs, lactation education and support, utilities payments/assistance all at one place.
References
Almeida, R. A., Dubay, L. C., & Ko, G. (2001). Access to care and use of health services by low-income women. Health Care Financing Review, 22(4), 27.
Centers for Disease Control and Prevention.(2017). Natality public-use data 2007-2015, on CDC WONDER Online Database. Retrieved from http://wonder.cdc.gov/natality-current.html
Centers for Disease Control and Prevention. (2015). 2015 Childhood combined 7-vaccine series coverage dashboard. Retrieved from https://www.cdc.gov/vaccines/imz-managers/coverage/childvaxview/data-reports/7-series/dashboard/2015.html
Centers for Disease Control and Prevention. (2013a). Preventive health care. Retrieved from
https://www.cdc.gov/healthcommunication/toolstemplates/entertainmented/tips/preventivehealth.html
Centers for Medicare & Medicaid Services. (2012). Emergency Medical Treatment & Labor Act (EMTALA). Retrieved from
https://www.cms.gov/Regulations-and-Guidance/Legislation/EMTALA/
Child Trends Databank. (2015). Immunization. Retrieved from
https://www.childtrends.org/indicators/immunization/
Escarce, J., & Kapur, K. (2006). Access to and quality of health care. Hispanics and the Future of America, 410-415.
Hagan, J. F., Shaw, J. S., & Duncan, P. M. (2007). Bright futures: Guidelines for health supervision of infants, children, and adolescents. Elk Grove Village, IL: American Academy of Pediatrics.
Office of Disease Prevention and Health Promotion. (2014). Maternal, infant, and child health. Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-child-health
San Antonio Metropolitan Health District. (2017). Strategic plan: January 2017 to December 2019. Retrieved from https://www.sanantonio.gov/Portals/0/Files/health/News/Reports/StrategicPlan5-25-2017.pdf?ver=2017-05-26-112910-987
Sunil, T. S., Spears, W. D., Hook, L., Castillo, J., & Torres, C. (2010). Initiation of and barriers to prenatal care use among low-income women in San Antonio, Texas. Maternal and Child Health Journal, 14(1), 133-140.
Texans Care for Children. (2016). Achieving healthy outcomes for moms and babies. Retrieved from https://static1.squarespace.com/static/5728d34462cd94b84dc567ed/t/5776af42579fb3c5c72b79df/1467395909147/testimony+birth+outcomes+hearing.+5.19.16.pdf
United Health Foundation. (2017). Spotlight: Prevention. Retrieved from http://cdnfiles.americashealthrankings.org/SiteFiles/PressReleases/FinalReport-SpotlightPrevention-26-Feb-2016.pdf
U.S. Department of Health and Human Services. (2014). Child health USA 2014. Retrieved from https://mchb.hrsa.gov/chusa14/health-services-financing-utilization/prenatal-care.html
U.S. National Library of Medicine. (2017). Prenatal care. Retrieved from https://medlineplus.gov/prenatalcare.html
Willis, E., Sabnis, S., Hamilton, C., Xiong, F., Coleman, K., Dellinger, M., ... & Nugent, M. (2016). Improving immunization rates through community-based participatory research: Community health improvement for Milwaukee’s children program. Progress in Community Health Partnerships: Research, Education, and Action, 10(1), 19-30.

C. HEALTHY EATING AND ACTIVE LIVING
Why is this important?
The two most important components to lead a healthy lifestyle include having a healthy diet and being physically active. Together, they can help individuals maintain a healthy weight and reduce their risks of having one or more chronic diseases such as heart disease and diabetes. Healthy eating and active living can therefore result in overall health (U.S. Department of Health & Human Services, 2017).
Results Statement
All Bexar County residents will flourish in a community that encourages healthy eating and active living.
Headline Indicators
-
Obesity in adults
-
Overweight in adults
Associated Indicators
-
Diabetes in adults
Story Behind the Baseline
Obesity is one of the most serious health threats facing our nation. Adults are overweight when they have a body mass index (BMI) between 25 kg/m2 and 29.9 kg/m2, and are obese when their BMI is of 30 kg/m2or greater (Office of the Surgeon General, 2001). According to the 2015 U.S. Behavioral Risk Factor Surveillance System Survey, 28.9% of American adults are obese and 35.5% are overweight (Centers for Disease Control and Prevention, 2015). The prevalence is higher among women than men, and racial and ethnic minority populations experience a greater burden of obesity compared to non-minority populations (Obesity Society, 2012).Obesity-related conditions such as heart disease and type 2 diabetes make up several of the leading causes of death in the U.S. (Centers for Disease Control and Prevention, 2017). Even a moderate weight excess such as an extra 10 to 20 pounds for a person of average height increases the risk of death (Calle, Thun, Petrelli, Rodriguez, & Heath, 1999). High rates of obesity are largely responsible for the rapidly rising healthcare costs in the nation (Centers for Disease Control and Prevention, 2017).
For the majority of individuals, obesity is caused by excessive caloric intake, a lack of availability and affordability of healthy foods, and an overwhelming deficiency in physical activity (Office of the Surgeon General, 2001). Regular physical activity can reduce the risk of obesity and chronic disease; even modest increases in activities such as walking and bicycling can help individuals lead longer, healthier lives (Public Health Law Center, 2017).
Texas ranks 8th in the nation for adult obesity (Trust for America’s Health, & Robert Wood Johnson Foundation, 2017). Data from 2015 show that 32.4% of adults in Texas were obese, and 36.3% of adults were overweight (Texas Department of State Health Services, 2015; Trust for America’s Health, & Robert Wood Johnson Foundation, 2017).
Bexar County is no exception to the alarming prevalence of obesity. In 2015, approximately 35.6percentof Bexar County adults were obese and 35.4% of adults were overweight (Texas Department of State Health Services, 2015). It is important to note that the Bexar County survey sample size in 2015 was small and had a lower statistical power than in 2014. The rates of both obese and overweight adults in Bexar County are expected to increase without additional intervention. By 2019, the partners that are working to decrease the obesity rate expect to reach a target of 32.4% obese adults in Bexar County. As the rate of obese adults decreases, they expect the rate of overweight adults to increase by 2019.
Several factors impact engagement in healthy eating and active living. At the individual level, Bexar County residents may refrain from eating healthy foods or engaging in physical activity because of their socioeconomic status measured by income and education (McLaren, 2007). In fact, a clinical BMI analysis of 67,000 unique Bexar County patients by zip code showed an association between BMI, income, and zip code (Healthcare Access San Antonio, 2017). Particularly for women, having a low income means they may not have the necessary resources to afford fruits and vegetables and would rather choose inexpensive, unhealthy food instead (Population Reference Bureau, 2010).Greater educational attainment also appears to be a protective factor for women, where women with college degrees are less likely to be obese compared to less educated women (Centers for Disease Control and Prevention, 2010).No such trend between obesity and education has been identified among men (Centers for Disease Control and Prevention, 2010).
Other factors affecting healthy eating and active living among individuals and their families may include specific mindsets toward food and physical activity norms, limited knowledge about the health benefits of these activities, and a lack of skills to cook and engaging in physical activity.
At a socio-ecological level (McLeroy, Bibeau, Steckler, & Glantz, 1988), individual choices and behaviors regarding healthy eating and active living are affected by the social and physical environments in which people live, including in the organizations where they function such as school and work, and in the broader community. A lack of safe places to be active (e.g., sidewalks, well-lit streets, or parks) can be important barriers for physical activity (Sallis, Floyd, Rodríguez, & Saelens, 2012). As a community, we must continue to create an environment that increases access to healthy foods and safe environments that promote physical activity
Prioritized Root Causes for the Community to Address
-
Lack of knowledge and skills of healthy eating and physical activity
-
Lack of safe places to be active within communities
-
Lack of financial security and affordability
-
Mindset of food and physical activity norms
Key Strategies
-
Improve infrastructure to reduce barriers to physical activity and healthy eating.
-
Promote a culture of healthy eating and active living at worksites, faith-based communities, schools, and neighborhoods.
-
Develop a coordinated system of screening for food insecurity.
-
Build relationships with businesses to invest and leverage resources for the health of the community (Health Impact Investing model).
References
Calle, E. E., Thun, M. J., Petrelli, J. M., Rodriguez, C., & Heath Jr, C. W. (1999). Body-mass index and mortality in a prospective cohort of US adults. New England Journal of Medicine, 341(15), 1097-1105.
Centers for Disease Control and Prevention. (2017). Adult obesity facts. Retrieved from https://www.cdc.gov/obesity/data/adult.html
Centers for Disease Control and Prevention. (2015). 2015 BRFSS Survey Data and Documentation. Retrieved from https://www.cdc.gov/brfss/annual_data/annual_2015.html
Centers for Disease Control and Prevention. (2010). Obesity and socioeconomic status in adults: United States, 2005-2008. Retrieved from https://www.cdc.gov/nchs/products/databriefs/db50.htm
Healthcare Access San Antonio. (2017). Analysis provided by Healthcare Access San Antonio.
McLaren, L. (2007). Socioeconomic status and obesity. Epidemiologic Reviews, 29(1), 29-48.
McLeroy, K. R., Bibeau, D., Steckler, A., & Glanz, K. (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15(4), 351-377.
Obesity Society. (2012). Obesity in US adults: 2012. Retrieved from
http://www.obesity.org/obesity/resources/facts-about-obesity/statistics
Office of the Surgeon General. (2001). The Surgeon General’s call to action to prevent and decrease overweight and obesity. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK44210/
Population Reference Bureau. (2010). For women in the U.S., obesity links to socioeconomic status and poor diet. Retrieved from
http://www.prb.org/Publications/Articles/2010/usobesity.aspx
Public Health Law Center. (2017). Active living. Retrieved from
http://www.publichealthlawcenter.org/topics/active-living
Sallis, J. F., Floyd, M. F., Rodríguez, D. A., & Saelens, B. E. (2012). Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation, 125(5), 729-737.
Texas Department of State Health Services. (2015). Texas Behavioral Risk Factor Surveillance System Survey Data. Austin, TX: Center for Health Statistics.
Trust for America’s Health, & Robert Wood Johnson Foundation. (2017). The state of obesity: Better policies for a healthier America. Retrieved from https://stateofobesity.org/states/tx/
U.S. Department of Health & Human Services (2017). Importance of good nutrition. Retrieved from https://www.hhs.gov/fitness/eat-healthy/importance-of-good-nutrition/index.html
D. SAFE COMMUNITIES
Why is this important?
Individuals and families have the right to grow and age in a healthy and secure environment, free of violence, abuse, and crime. Feeling secure in one’s social and physical environment can lead to ongoing participation in work, leisure and educational opportunities, and ultimately a positive state of well-being and high quality of life (Safe Communities Foundation, 2015).
Results Statement
Bexar County will be recognized as one of the safest places to live, work, play, and thrive for all.
Headline Indicators
-
Crime rates as measured by:
-
Violent crime
-
Family violence crime
-
Child abuse and neglect crime
-
-
Traffic fatalities
Associated Indicators
-
Homicide age-adjusted death
-
Non-natural crude death
Story Behind the Baseline
Poverty, defined as a lack of economic resources, can have negative social consequences (Mood & Jonsson, 2016). Poverty may limit access to higher education or employment opportunities (Barr, 2008). Individuals and families living in poverty may experience generational stress and trauma, which can negatively impact their physical and mental health. They may engage in risky behaviors such as substance abuse or risky driving, such as driving over the speed limit. They may feel socially discriminated against or excluded, and may even engage in violence and crime (Duncan & Magnuson, 2011; Macartney, Bishaw, & Footenot, 2013; Oesterle et al., 2004). As families living in poverty have less access to resources to successfully adapt to their circumstances, trauma and violence are often perpetuated over time including through adverse childhood experiences, and intimate partner violence. Evidence suggests that the higher the poverty and unemployment rates, the higher the crime activity in the community (Hooghe, Vanhoutte, Hardyns, & Bircan, 2010). A safe community can therefore be measured by specific crime rates and traffic fatalities.
Crimes
Three specific types of crimes are of interest: violent crimes, family violence crimes, and child abuse and neglect crimes. Violent crimes are crimes where a perpetrator uses force or threat of force upon a victim and commits murder, rape, robbery, or aggravated assault (U.S. Department of Justice, 2012). Family violence crimes are incidents between family or household members (i.e., spouses, parents, children, or any other individuals above the age of 18 related by blood or marriage) that cause physical injury, such as assaults, homicides, kidnapping and abductions, sex offenses, and robbery (Connecticut General Assembly, 2009). Child abuse and neglect crimes are any act or failure to act on the part of a parent or caretaker, which results in death, serious physical, sexual, and emotional abuse, medical and physical neglect, and abandonment of a person 17 years of age or under (U.S. Department of Health & Human Services, 2016).
Across the United States, in 2015, there were 372.6 violent crimes per 100,000 population (Federal Bureau of Investigation, 2015), representing a total of close to 1.2 million violent crimes in one year. In 2016 in Texas, the same crime rate was 432.8 per 100,000 population (Texas Department of Public Safety, 2016). In 2016 Bexar County, the rate was 608 crimes per 100,000 population (Texas Department of Public Safety, 2016); this is 1.4 times higher than the 2016 Texas rate and 1.6 times higher than the 2015 US rate. The Bexar County rate is expected to slightly increase without additional intervention.
National data on family violence crimes and child abuse and neglect crimes are not common, with the last report on family violence crimes from the U.S. Department of Justice published in 2005. At that time, children were included in the rate and there were 2.1 victims per 1,000 U.S. residents age 12 or older (U.S. Department of Justice, 2005). Today, minors are considered under the child abuse and neglect crimes. In 2012 in the U.S., the rate was 9.2 per 1,000 children were victims of child abuse and neglect crimes (Centers for Disease Control and Prevention, 2014). Among those, 1,640 children died from child maltreatment at a rate of 2.2 per 100,000 children (Centers for Disease Control and Prevention, 2014). Despite these numbers, a large percentage of crimes are not reported to authorities in the hopes of protecting the perpetrator or the victim (U.S. Department of Justice, 2005).
The Texas family violence rate in 2015 was 709 crimes per 100,000 population (Texas Department of Public Safety, 2015). In 2015 in Bexar County, the rate was 809 per 100,000 population (Texas Department of Public Safety, 2015), 14% higher than the Texas rate. The Bexar County rate is expected to slightly increase without additional intervention.
In 2016 in Texas, the child abuse and neglect crimes rate was 7.9 crimes for every 1,000 children(Texas Department of Family and Protective Services, 2016).In Bexar County in 2016, this rate was 9.0 per 1,000 children (Texas Department of Family and Protective Services, 2016); this is 14% higher than Texas. The Bexar County rate is expected to slightly increase without additional intervention.
Traffic Fatalities
Along with crimes, risky driving leading to traffic fatalities also makes our communities unsafe. Risky driving is defined as drunk, drugged, distracted, or drowsy driving, speeding, and not wearing seat belts (National Highway Traffic Safety Administration, 2017). Traffic fatalities can be caused by several factors, including risky driving, road design, and other external factors. Traffic fatalities are defined as deaths from crashes on public roads where at least one vehicle with an engine was involved, and at least one person died within 30 days as a result of the crash (National Highway Traffic Safety Administration, 2015). This could include, a pedestrian being hit by a bus, a motorcyclist losing control of his vehicle and colliding into a tree, or a crash between two vehicles.
In the United States, a total of 35,092 people died in motor vehicle crashes in 2015, representing 10.9 deaths per 100,000 population (National Highway Traffic Safety Administration, 2015; San Antonio Metropolitan Health District, 2017). In 2016 in Texas, the rate of traffic fatalities was 13.5 per 100,000 population, which is slightly higher than the 2015 national average (Texas Department of Transportation, 2016; San Antonio Metropolitan Health District, 2017).Comparatively, in Bexar County in 2016, the rate of traffic fatalities was 11.4 deaths per 100,000 population (San Antonio Metropolitan Health District, 2017; (Texas Department of Transportation, 2016), which is 18% lower than the 2016 Texas rate and 5% higher than the 2015 U.S. rate. The Bexar County rate increased by 33% from 2011 to 2016. The Bexar County rate is expected to increase without additional intervention.
Concerns in Bexar County
Considering that poverty is one of the core components that shapes and determines a community’s safety, and that crime and traffic fatalities can both represent community safety and be a symptom of poverty, we will aim to make Bexar County safer by addressing both poverty and its symptoms. It is by resolving issues related to poverty and other systematic root causes that we may begin to alleviate problems of violence.
As a historically and socially stratified county by race/ethnicity and class, focus must be on increasing access to political and social resources in low-income neighborhoods, as well as investing in public infrastructure and places with community character that enhance safety and livability. For example, investments in road design including sidewalks, lighting, and safe streets for pedestrians and bicyclists could help decrease motor vehicle accidents at intersections (Morency, Gauvin, Plante, Fournier, & Morency, 2012). Simultaneously, building and revitalizing social capital and a sense of belonging among community members while working for the greater good could help increase a perceived order and sense of security, which could decrease crimes and fear of crimes (Scarborough, Like-Haislip, Novak, Lucas, & Alarid, 2010).
Prioritized Root Causes for the Community to Address
-
Lack of, or insufficient, educational and economic opportunities
-
Lack of quality infrastructure and places with community character that enhance safety and livability and moves beyond providing only minimum safety standards
-
History of trauma (e.g., intergenerational, adverse childhood events, from violence)
Key Strategies
-
Increase opportunities and education that address systemic root causes of violence and intergenerational poverty.
-
Increase and improve infrastructure and places in the areas with the most need.
-
Provide intervention programs that break the cycle of trauma and promote trauma-informed care.
References
Barr, D. A. (2008). Health disparities in the United States: Social class, race, ethnicity, and health. Baltimore, MD: Johns Hopkins University Press.
Bexar County Community Health Collaborative. (2016). Bexar County Community Health Needs Assessment. Retrieved from http://healthcollaborative.net/wp-content/uploads/reports/chna-2016.pdf
Centers for Disease Control and Prevention. (2014). Child maltreatment. Retrieved from https://www.cdc.gov/violenceprevention/pdf/childmaltreatment-facts-at-a-glance.pdf
Connecticut General Assembly. (2009). Summary of family violence laws. Retrieved from https://www.cga.ct.gov/2009/rpt/2009-R-0349.htm
Duncan, G. J., & Magnuson, K. (2011, winter). The long reach of early childhood poverty. Pathways: A Magazine on Poverty, Inequality, and Social Policy, 22–27.
Federal Bureau of Investigation. (2015). Crime in the United States. Retrieved from https://ucr.fbi.gov/crime-in-the-u.s/2015/crime-in-the-u.s.-2015/tables/table-1
Hooghe, M., Vanhoutte, B., Hardyns, W., & Bircan, T. (2010). Unemployment, inequality, poverty and crime: spatial distribution patterns of criminal acts in Belgium, 2001–06. The British Journal of Criminology, 51(1), 1-20.
Insurance Institute for Highway Safety & Highway Loss Data Institute. (2015). Yearly snapshot. Retrieved from http://www.iihs.org/iihs/topics/t/general-statistics/fatalityfacts/overview-of-fatality-facts
Macartney, S., Bishaw, A., & Fontenot, K. (2013). Poverty rates for selected detailed race and Hispanic groups by state and place: 2007-2011. US Department of Commerce, Economics and Statistics Administration, US Census Bureau.
Morency, P., Gauvin, L., Plante, C., Fournier, M., & Morency, C. (2012). Neighborhood social inequalities in road traffic injuries: the influence of traffic volume and road design. American Journal of Public Health, 102(6), 1112-1119.
National Highway Traffic Safety Administration. (2017). Risky driving. Retrieved from https://www.nhtsa.gov/risky-driving
National Highway Traffic Safety Administration. (2015). Traffic safety facts 2015 report. Retrieved from https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/812384
Oesterle, S., Hill, K. G., Hawkins, J. D., Guo, J., Catalano, R. F., & Abbott, R. D. (2004). Adolescent heavy episodic drinking trajectories and health in young adulthood. Journal of Studies on Alcohol, 65(2), 204-212.
Safe Communities Foundation. (2015). A safe community is a real community. Retrieved from http://www.safecommunities.org.nz/become-safe-community/benefits-being-safe-community
San Antonio Metropolitan Health District. (2017). Analysis provided by the local health department.
Scarborough, B. K., Like-Haislip, T. Z., Novak, K. J., Lucas, W. L., & Alarid, L. F. (2010). Assessing the relationship between individual characteristics, neighborhood context, and fear of crime. Journal of Criminal Justice, 38(4), 819-826.
Texas Department of Family and Protective Services. (2016). CPS investigations: Victims. Retrieved from https://www.dfps.state.tx.us/About_DFPS/Data_Book/
Child_Protective_Services/Investigations/Victims.asp
Texas Department of Public Safety. (2016). Texas crime report: 2016 crime in Texas: Executive summary. Retrieved from http://www.dps.texas.gov/crimereports/16/executiveSummary.pdf
Texas Department of Public Safety. (2015). Texas crime report: Chapter 5: Family violence. Retrieved from
https://www.dps.texas.gov/crimereports/15/citCh5.pdf
Texas Department of Transportation. (2016). Crashes and injuries by county. Retrieved from http://ftp.dot.state.tx.us/pub/txdot-info/trf/crash_statistics/2016/12.pdf
The Borgen Project. (2014). Fiveeffects of poverty. Retrieved from https://borgenproject.org/5-effects-poverty/
U.S. Department of Health & Human Services. (2016). Definitions of child abuse and neglect in federal law. Retrieved from https://www.childwelfare.gov/topics/can/defining/federal/
U.S. Department of Justice. (2012). Violent crime. Retrieved from https://ucr.fbi.gov/crime-in-the-u.s/2011/crime-in-the-u.s.-2011/violent-crime/violentcrimemain_final.pdf
U.S. Department of Justice. (2005). Family violence statistics including statistics on strangers and acquaintances. Retrieved from https://www.bjs.gov/content/pub/pdf/fvs05.pdf






E. SEXUAL HEALTH
Why is this important?
Sexual health can lead to a state of physical, emotional, mental and social well-being in relation to sexuality. Preventing unintended consequences such as unwanted pregnancies and sexually transmitted diseases, as well as seeking sexual health information, education, treatment, and care can promote sexual health and healthy relationships (American Sexual Health Association, 2017).
Results Statement
The Bexar County community will be sexually healthy without abuse, disease, or stigma.
Headline Indicators
-
Incidence of sexually transmitted diseases as measured by:
-
HIV
-
Chlamydia
-
Gonorrhea
-
Syphilis
-
Associated Indicators
-
Teen birth rates
-
HPV Vaccinations in teens
Story Behind the Baseline
Sexually transmitted diseases (STD) are infections spread from person to person through sexual contact such as vaginal, oral, or anal sex (Office on Women’s Health, 2017). The most common STDs are chlamydia, gonorrhea, hepatitis B virus, herpes simplex virus type 2, human immunodeficiency virus (HIV), human papillomavirus (HPV), syphilis, and trichomoniasis (Centers for Disease Control and Prevention, 2013). In the United States, close to 20 million new STDs occur every year, with half of new cases being among people age 15 to 24 years old (Centers for Disease Control and Prevention, 2016a). Each infection can have immediate and long-term effects on the health and well-being of the person infected, including causing infertility and chronic pain (Centers for Disease Control and Prevention, 2016a). It is also common for individuals to get more than one concurrent STD (Choudhry, Ramachandran, Das, Bhattacharya, & Mogha, 2010). Having an STD can also make it easier to acquire another STD, such as HIV (Centers for Disease Control and Prevention, 2017a).
Rates of STDs are increasing at an alarming rate. Approximately 1.2 million people in the United States are living with HIV (Centers for Disease Control and Prevention, 2016b). There were 39,393 new HIV infections diagnosed in 2015, representing 12.3 per 100,000 population (Centers for Disease Control and Prevention, 2016c). Gay, bisexual, and other men who have sex with men experience the greatest burden of this disease (Centers for Disease Control and Prevention, 2016b). In Texas, an estimated 4,476 adults and adolescents were diagnosed with HIV in 2015, ranking Texas as the state with the 3rd highest incidence of new HIV diagnoses in the country (Centers for Disease Control and Prevention, 2016c). This incidence represents 16.1 diagnoses per 100,000 population (Texas Department of States and Human Services, 2017). In Bexar County, there were 19.1 new HIV infections diagnosed per 100,000 population in 2015 (San Antonio Metropolitan Health District, 2017); Bexar County’s 2015 rate is 1.6 times the U.S. rate and 1.2 times the Texas rate. The rate in Bexar County is expected to increase without additional intervention. By 2019, the partners that are working together to decrease this rate expect it to fall to 18.8 per 100,000 population.
In terms of other STDs, nearly 1.6 million cases of chlamydia were reported across the United States in 2016 alone (Centers for Disease Control and Prevention, 2017b). This represented 497.3 cases per 100,000 individuals, or a 4.7 percent increase since 2015 (Centers for Disease Control and Prevention, 2017b). In 2015 in Texas, there were 486 cases of chlamydia per 100,000 population (Texas Health and Human Services, 2016). Yet in Bexar County there were 689 cases of chlamydia per 100,000 population (San Antonio Metropolitan Health District, 2017), which is 1.4 times both the national and Texas rates. The rate in Bexar County is expected to slightly increase without additional intervention. By 2019, the partners that are working to decrease this rate expect it to fall to 633 per 100,000 population.
Cases of gonorrhea increased by 19.6% from 2015 to 2016 for a rate of 135.6 per 100,000 individuals (Centers for Disease Control and Prevention, 2017c).In 2015 in Texas, there were 137 cases per 100,000 population (Texas Health and Human Services, 2016). In Bexar County there were 206 cases per 100,000 population(San Antonio Metropolitan Health District, 2017), 1.7 times the national rate and 1.5 times the Texas rate. The rate in Bexar County is expected to slightly increase without additional intervention. By 2019, the partners that are working to decrease this rate expect it to fall to 181 per 100,000 population.
Total syphilis cases reported in the U.S. also increased by 17% from 2014 to 2015 to a rate of 23.2cases per 100,000 population (Centers for Disease Control and Prevention, 2016a). In 2015 in Texas, there were 30.6 cases per 100,000 people(Texas Health and Human Services, 2016). In Bexar County there were 48.9 cases per 100,000 population(San Antonio Metropolitan Health District, 2017), which represents 2.1 times the national rate and 1.6 times the Texas rate. The rate in Bexar County is expected to increase without additional intervention. By 2019, the partners that are working to decrease this rate expect it to fall to 48.9 per 100,000 population.
A large number of factors have been shown to influence the rates of STDs in our community. At the individual level, lack of education and prevention can lead to risky sexual behaviors, multiple sex partners, and unprotected sex(Centers for Disease Control and Prevention, 2016a; Institute of Medicine Committee on Prevention and Control of Sexually Transmitted Diseases, 1997).Social and cultural factors play an important role in STD prevalence such as the presence of social stigma around STDs as well as difficulty accessing health care and other community resources (Centers for Disease Control and Prevention, 2016b; Institute of Medicine Committee on Prevention and Control of Sexually Transmitted Diseases, 1997). In fact, cases go undiagnosed because individuals are uninsured or cannot afford copayments and deductibles (Institute of Medicine Committee on Prevention and Control of Sexually Transmitted Diseases, 1997) or because some STD have no symptoms or the symptoms resolve on their own, so individuals do not seek treatment (Centers for Disease Control and Prevention, 2016c).
Several community partners have led significant work in the past five years to address STDs in our community. Interventions have included expanded testing for the public, increased condom distribution, case management for pregnant women, and mobile clinics to reach areas in San Antonio that have high incidence of disease. Policies such as the October 2015 mandatory screenings for syphilis among pregnant women during the third trimester have also had an influence. Community partners continue to work together on outreach events to educate and raise awareness. Although a large amount of work has been done in this area, Bexar County rates remain above Texas and U.S. rates for all four headline indicators, suggesting that interventions to address the root causes of these STDs are needed. In other words, more collaboration is needed to help educate about prevention, elevate awareness of community resources, as well as address barriers such as stigma and access to health care.
Prioritized Root Causes for the Community to Address
-
Culture and presence of stigma in the community
-
Lack of preventive care and education
-
Lack of access to health care and resources
Key Strategies
-
Increase education (to include stigma and abuse) with improved collaboration and coordination within Bexar County.
-
Increase access to condoms.
-
Increase STD prevention, testing, and treatment, including identification of those who test but do not provide treatment.
References
American Sexual Health Association. (2017). Understanding sexual health. Retrieved from http://www.ashasexualhealth.org/sexual-health/
Centers for Disease Control and Prevention. (2013). Incidence, prevalence, and cost of sexually transmitted infections in the United States. Retrieved from https://www.cdc.gov/std/stats/sti-estimates-fact-sheet-feb-2013.pdf
Centers for Disease Control and Prevention. (2017b). Chlamydia. Retrieved from https://www.cdc.gov/std/stats16/chlamydia.htm
Centers for Disease Control and Prevention. (2017c). Gonorrhea. Retrieved from https://www.cdc.gov/std/stats16/Gonorrhea.htm
Centers for Disease Control and Prevention. (2017a). STDs and HIV – CDC Fact Sheet. Retrieved from https://www.cdc.gov/std/hiv/stdfact-std-hiv.htm
Centers for Disease Control and Prevention. (2016a). Today’s HIV/AIDS epidemic. Retrieved from https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/todaysepidemic-508.pdf
Centers for Disease Control and Prevention. (2016b). Texas – State health profile. Retrieved from https://www.cdc.gov/nchhstp/stateprofiles/pdf/texas_profile.pdf
Centers for Disease Control and Prevention. (2016d). CDC fact sheet: information for teens and young adults staying healthy and preventing STDs. Retrieved from https://www.cdc.gov/std/life-stages-populations/stdfact-teens.htm
Choudhry, S., Ramachandran, V. G., Das, S., Bhattacharya, S. N., & Mogha, N. S. (2010). Characterization of patients with multiple sexually transmitted infections: A hospital-based survey. Indian Journal of Sexually Transmitted Diseases, 31(2), 87.
Institute of Medicine Committee on Prevention and Control of Sexually Transmitted Diseases. (1997). Factors that contribute to the hidden epidemic. In T. R. Eng, & Butler, W. T. (Eds). The Hidden Epidemic: Confronting Sexually Transmitted Diseases. Washington, DC: National Academies Press.
San Antonio Metropolitan Health District. (2017). Analysis provided by the local health department.
Office on Women’s Health. (2017). Sexually transmitted infections. Retrieved from https://www.womenshealth.gov/a-z-topics/sexually-transmitted-infections
Texas Department of States and Human Services. (2017). Texas HIV surveillance report. Retrieved from https://www.dshs.texas.gov/hivstd/reports/HIVSurveillanceReport.pdf
Texas Health and Human Services. (2016). Texas STD surveillance report. Retrieved from https://dshs.texas.gov/hivstd/reports/STDSurveillanceReport.pdf




